Why Dental Recall Systems Fail (And How to Fix Yours)
Posted on 2/16/2026 by WEO Media |
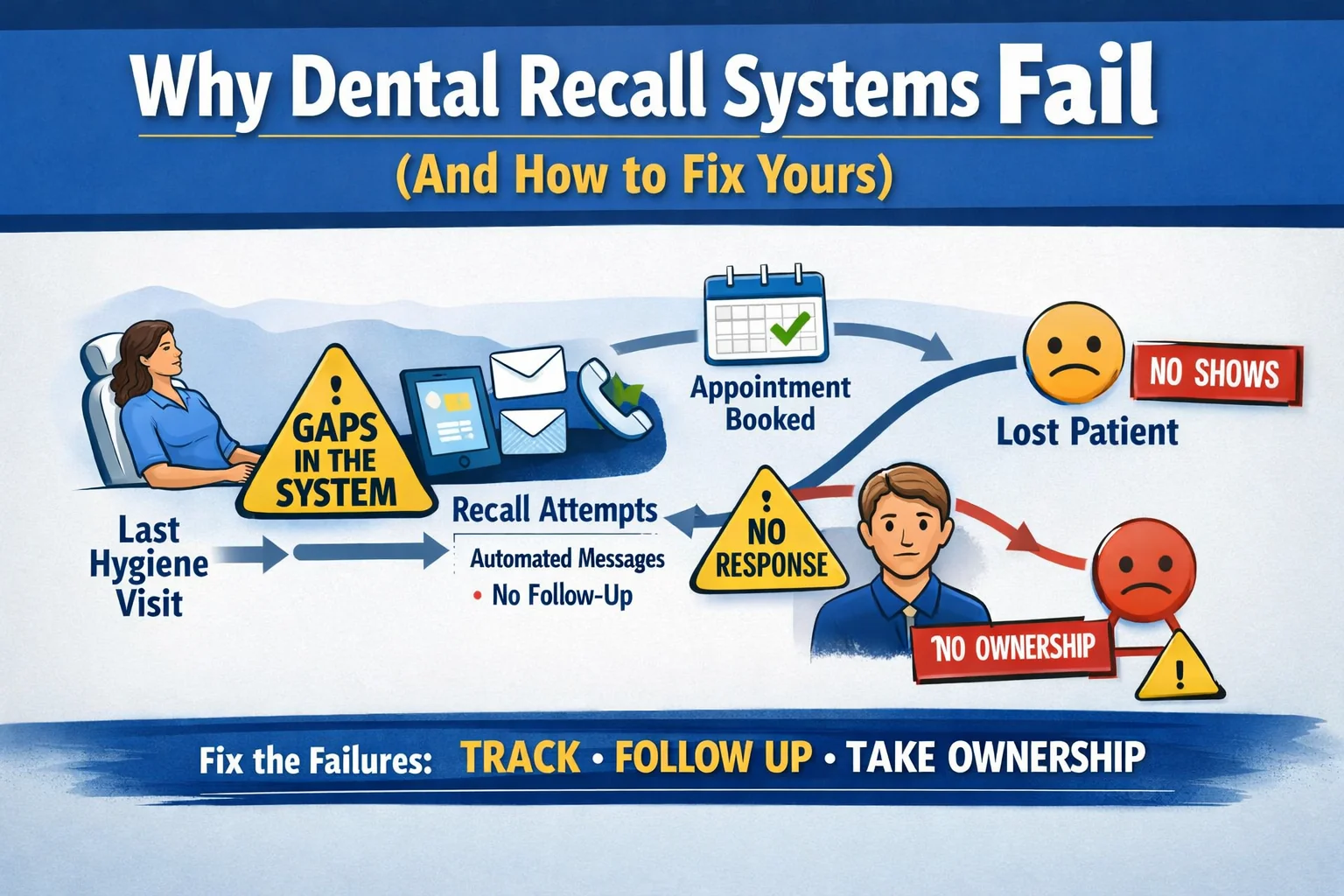
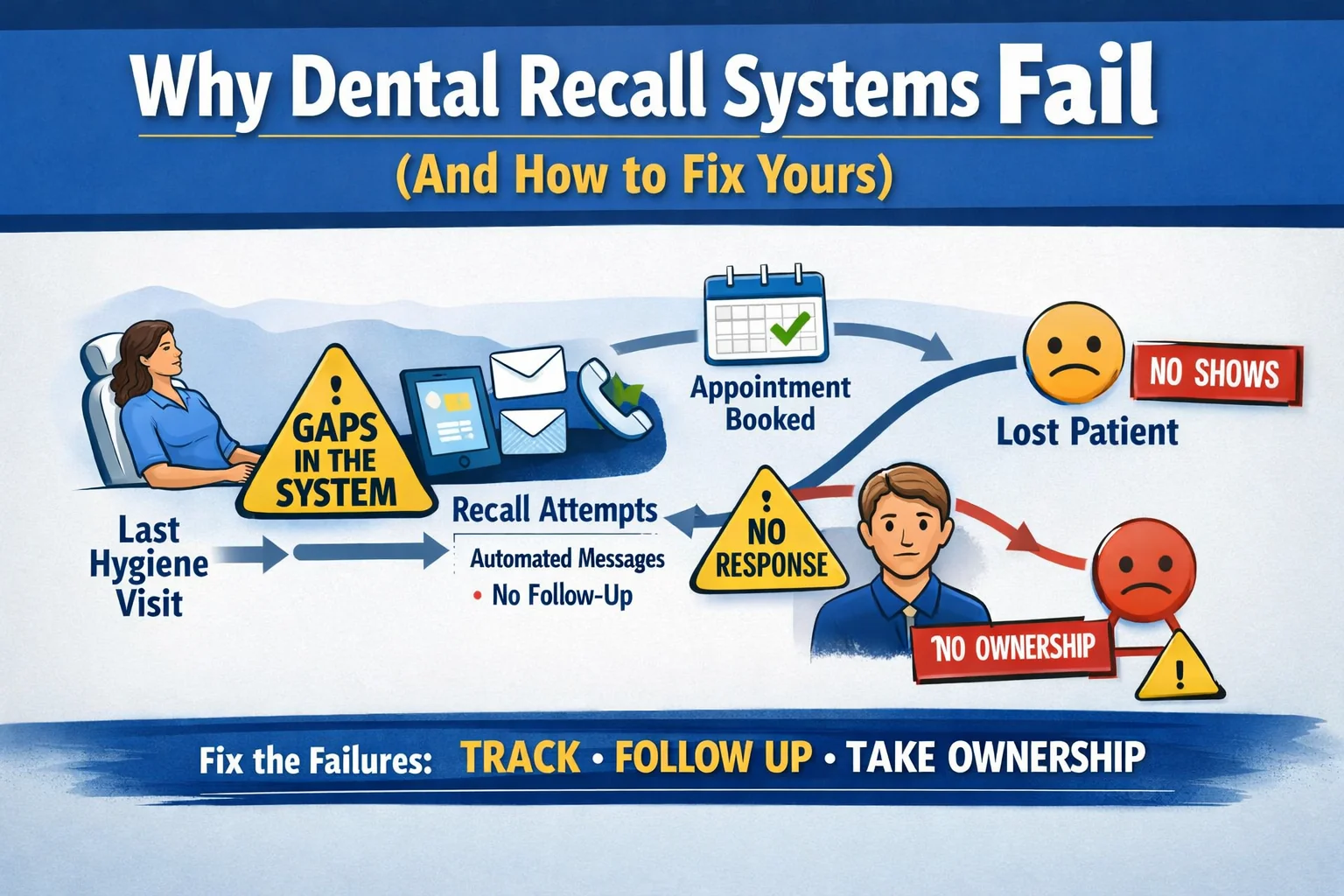 Dental recall systems fail when the process runs on autopilot and nobody watches what happens after the message goes out. Most dental practices have some version of a recall process: automated texts, postcards, maybe a phone call list. But having a recall system and having one that actually converts overdue patients into kept appointments are two different things. If your hygiene schedule has open holes, your recare percentage is slipping, or your “past due” patient list keeps growing, the problem almost certainly isn’t that patients forgot about you. It’s that your patient pipeline has gaps between the reminder and the kept appointment. Dental recall systems fail when the process runs on autopilot and nobody watches what happens after the message goes out. Most dental practices have some version of a recall process: automated texts, postcards, maybe a phone call list. But having a recall system and having one that actually converts overdue patients into kept appointments are two different things. If your hygiene schedule has open holes, your recare percentage is slipping, or your “past due” patient list keeps growing, the problem almost certainly isn’t that patients forgot about you. It’s that your patient pipeline has gaps between the reminder and the kept appointment.
The pattern is consistent across practices we work with: recall messages fire on schedule, but no one tracks whether those messages actually lead to booked appointments. The reminders become background noise—patients receive them, ignore them, and drift further from the practice. Meanwhile, the front desk assumes “the system is handling it” while the schedule tells a different story. Whether your patients originally came from SEO, paid ads, or referrals, losing them at the recall stage wastes every dollar you spent to acquire them. The core failures are timing gaps, single-channel dependence, no human follow-up, unclear ownership, and no measurement of what actually converts. These are workflow problems, not technology problems—and they’re fixable without replacing your software.
If your recall volume is healthy but patients aren’t booking, keep reading. If you need more new patients first, start with patient acquisition strategies.
Below, you’ll learn how to audit your current recall system using real numbers (sent → opened → responded → booked → kept), identify which of the five most common failure points is costing you patients, and fix each one with specific workflow changes, timing adjustments, scripts your team can use immediately, and a simple tracking method that turns guesswork into data—without expensive new software or blame.
Written for: dental practice owners, office managers, and hygiene coordinators who have a recall system in place but aren’t seeing it translate into a consistently full hygiene schedule.
TL;DR
If you only fix five things in your recall system, fix these:
| • |
Measure what actually happens after reminders send — track sent → opened → responded → booked → kept so you can see exactly where patients drop off
|
| • |
Add a human follow-up step for non-responders — automated messages alone convert a fraction of overdue patients; a personal call within 48 hours of no response changes the math
|
| • |
Use the right channel at the right time — text for the first reminder, call for the second attempt, and a personal outreach for patients 60+ days overdue
|
| • |
Assign one person to own recall outcomes — shared responsibility means no one tracks whether the overdue list is actually shrinking
|
| • |
Shorten the gap between “due” and “first contact” — reaching patients 2–4 weeks before their due date converts significantly better than contacting them after they’re already overdue |
Table of Contents
Why most dental recall systems quietly underperform
Most recall systems aren’t broken in an obvious way. They send messages. Patients receive them. The software dashboard shows activity. But the hygiene schedule still has gaps, and the overdue patient list grows by a few names every week. The failure is quiet—which is exactly why it persists.
A pattern we commonly see: a practice sets up automated recall when they first adopt their practice management software. The defaults fire a text or email at set intervals—30 days before, 7 days before, day of. The system appears to be working because messages are going out. But no one ever closes the loop to ask: of the 200 recall messages we sent last month, how many turned into kept appointments?
The answer, in most practices we audit, is surprisingly low. Automated reminders alone typically convert between 20–40% of the patients they reach. That means 60–80% of your overdue patients are receiving messages, doing nothing, and quietly drifting away from your practice. Without a human follow-up layer and a way to track outcomes by channel, the system creates the appearance of recall management while patients leave through the back door.
There are also structural issues that undermine recall before a single message sends. If your scheduling doesn’t pre-appoint patients at checkout (booking their next hygiene visit before they leave), your recall system starts from a deficit. Pre-appointment rates below 70% mean your recall list is artificially large—full of patients who should have been scheduled before they ever became “due.” This is a front desk process problem that no amount of recall automation will solve.
> Back to Table of Contents
How to measure your recall system’s real performance
If you suspect your recall system is underperforming but can’t prove it, run this simple audit over one month. You need five numbers, and most practice management systems can generate them with a basic report. Understanding where patients drop off in your marketing funnel is the key to fixing the right problem.
The recall conversion funnel: sent → opened → responded → booked → kept. Each step reveals a different type of problem.
| • |
Sent — total recall messages sent in the period (texts, emails, postcards, calls); if this number is low relative to your overdue list, messages aren’t firing correctly or patient contact info is outdated
|
| • |
Opened/delivered — for emails, check open rates; for texts, check delivery confirmations; texts generally have very high read rates, so if patients still aren’t responding, the message content or timing is the issue rather than delivery
|
| • |
Responded — patients who took any action (replied, clicked a link, called back); a big drop from opened to responded usually means the message doesn’t make it easy to act
|
| • |
Booked — patients who actually scheduled an appointment; a drop here often points to friction in the booking process itself (hold times, limited availability, no online scheduling option)
|
| • |
Kept — patients who showed up; a gap between booked and kept reveals a confirmation or day-of communication issue |
How to calculate your recall effectiveness rate: divide kept appointments by total recall messages sent, then multiply by 100. For example, if you sent 300 recall messages last month and 75 patients kept their recare appointment, your recall effectiveness rate is 25%. That gives you a single number to track monthly and a clear target to improve.
What we typically find: practices that rely solely on automated messages see effectiveness rates between 15–30%. Adding a structured human follow-up step for non-responders typically pushes that into the 40–55% range. The difference is meaningful—in a practice sending 300 recall messages per month, moving from 25% to 45% effectiveness means 60 additional kept hygiene appointments per month. If you need help connecting these numbers to your broader practice metrics, start by tracking this single recall rate alongside your other KPIs.
> Back to Table of Contents
The five recall failures that cost you patients (and how to fix each one)
After auditing recall systems across hundreds of dental practices, the same five failures appear repeatedly. Each one is fixable with workflow changes—not new software.
Failure 1: Timing is off
The most common timing mistake is reaching out after a patient is already overdue rather than before. Once a patient passes their due date without hearing from the practice, they mentally deprioritize the visit. Every additional week of silence makes reactivation harder.
The fix: shift your first recall contact to 2–4 weeks before the due date, not after it. Structure your sequence as a countdown: first message at 28 days before, second at 14 days before, third at 7 days before. If the patient doesn’t respond by the due date, that triggers the human follow-up call. This simple shift moves the system from reactive (chasing overdue patients) to proactive (filling the schedule before gaps appear).
Failure 2: Single-channel dependence
Many practices rely on one channel—usually automated texts—for all recall communication. The problem is that patients who don’t respond to texts won’t respond to more texts. Sending the same type of message three or four times just trains patients to ignore it. Following SMS best practices helps, but texts alone aren’t enough for a complete recall strategy.
The fix: vary the channel across your recall sequence. A practical pattern that works well: first contact via text (highest open rate for routine reminders), second via automated email sequences (allows more context and a direct booking link), third via phone call (personal touch for patients who haven’t responded to digital). For patients who are 60+ days overdue, a brief personal outreach—“We noticed you’re due and wanted to check in”—converts significantly better than another automated blast.
Failure 3: No human follow-up layer
This is the single biggest gap in most recall systems. Automated messages handle the easy wins—patients who were already planning to schedule. The harder-to-reach patients (and there are always more of them) need a person. Without a defined human follow-up step, those patients simply fall through.
The fix: build a “non-responder” workflow. After your automated sequence completes (typically 2–3 messages over 3–4 weeks), any patient who hasn’t booked goes onto a call list. Assign one team member to own that list. Set a target: call within 48 hours of the last automated message. Track the outcome of each call (booked, callback scheduled, declined, unreachable). This turns “the system handles it” into “we handle what the system can’t.” If you want a framework for documenting these steps, our guide to dental marketing SOPs covers how to build repeatable workflows your team can follow consistently.
Failure 4: No clear ownership
When recall is “everyone’s job,” it’s effectively no one’s job. In practices without a named recall owner, the overdue list grows quietly because no single person is accountable for whether it shrinks. The front desk assumes the hygienists are following up. The hygienists assume the front desk is calling. Nobody checks.
The fix: assign one person as the recall owner. This person doesn’t have to make every call, but they own the metric. They review the overdue list weekly, ensure follow-up calls are happening, and report on recall effectiveness in team meetings. In our experience, simply naming an owner—without changing anything else—improves recall rates measurably within 30 days because someone is finally watching the numbers. Pairing ownership with a documented playbook—what gets reviewed, how often, and what the escalation path is—makes this shift stick, because the owner has clear expectations rather than guessing at what “owning recall” means day to day.
Failure 5: No measurement of what converts
Most practices track how many recall messages they send but not how many convert to kept appointments. Without that closed-loop measurement, you can’t tell whether your system is working, which channels perform best, or whether changes you make actually improve anything. You’re running the system on faith.
The fix: track the full funnel (sent → opened → responded → booked → kept) monthly. Use the recall effectiveness rate (kept ÷ sent × 100) as your primary metric. Review it in a 10-minute weekly huddle. When you see a drop between specific stages, that tells you exactly where to focus. A drop from opened to responded means your message content needs work. A drop from responded to booked means your scheduling process has friction. Data replaces debate.
> Back to Table of Contents
How to build a recall workflow that reactivates patients
A complete recall workflow has three layers: pre-appointment (before the patient leaves), automated outreach (digital reminders), and human follow-up (personal contact for non-responders). Most practices have pieces of this but rarely all three working together. If you’re also looking at broader patient reactivation campaigns, this recall workflow is the foundation everything else builds on.
Layer 1: Pre-appointment at checkout
The best recall system is one you barely need. When a patient pre-books their next hygiene visit before leaving the office, they never enter the recall cycle at all. Target a pre-appointment rate of 80% or higher. If your rate is below 70%, fixing this single step will reduce your overdue list faster than any recall technology.
How to improve pre-appointment rates: make it the default, not the exception. Train hygienists to say “Let’s get your next visit on the calendar before you head out” at the end of every appointment. Give the front desk a simple script: “Dr. [Team] would like to see you back in six months. I have [date] at [time] or [date] at [time]—which works better for you?” Offering two specific options converts better than “Would you like to schedule your next appointment?” Understanding the patient journey from appointment to rebooking helps your team see why this moment matters so much.
Layer 2: Automated outreach sequence
For patients who don’t pre-book (or who cancel), the automated sequence should activate on a clear timeline:
| • |
28 days before due date — appointment text reminder: friendly, short, includes a direct booking link or “reply YES to schedule”
|
| • |
14 days before due date — reactivation email: slightly more context, mentions why the visit matters (“staying on track with your cleaning schedule”), includes online scheduling link
|
| • |
7 days before due date — text message: gentle urgency (“Your hygiene visit is coming up—we’d love to get you on the schedule”)
|
| • |
Due date + 3 days (if no response) — triggers the human follow-up list |
Key detail: every automated message should make booking as frictionless as possible. If a patient has to call during business hours to schedule, you’ll lose a large portion of people who read the message at night or on weekends. An online appointment scheduling link or a “reply to book” option significantly improves response rates. The question of what to automate versus what needs a human touch is central to getting this balance right.
Layer 3: Human follow-up for non-responders
This is where most of your recoverable patients live. The call doesn’t need to be long or complicated—30 to 60 seconds is enough. The goal is to connect personally and remove friction.
Workflow for the recall owner:
| 1. |
Pull the non-responder list — patients whose automated sequence completed with no booking (review daily or every other day)
|
| 2. |
Call within 48 hours — the sooner after the last automated message, the better; the patient still has the reminder in mind
|
| 3. |
Log the outcome — booked, callback scheduled (with specific date/time), declined, or unreachable
|
| 4. |
Follow up on callbacks — if a patient said “call me next week,” that callback has a named owner and a due date
|
| 5. |
Close out after three attempts — if three calls over two weeks produce no response, move the patient to a 90-day reactivation list rather than calling indefinitely |
This structure prevents the two most common follow-up failures: calls that never happen (because no one owns them) and calls that loop forever (because there’s no close-out rule).
> Back to Table of Contents
When the problem isn’t really recall
Sometimes a recall system underperforms not because of the system itself but because of upstream issues that create an artificially large overdue population. Before overhauling your recall workflow, check for these:
| • |
Low pre-appointment rates — if fewer than 70% of hygiene patients book their next visit at checkout, your recall system is doing work that should have been handled at the chair; fix pre-appointment first
|
| • |
Scheduling friction — if patients respond to recall messages but don’t book, the problem is usually limited hygiene availability, long hold times, or no online scheduling option; your recall system is generating demand that the schedule can’t absorb
|
| • |
Outdated contact information — if your sent-to-opened ratio is very low, messages may be going to old phone numbers or email addresses; a quarterly contact info verification at check-in solves this gradually
|
| • |
Patient experience issues — if patients are reached, book, and then don’t return, the problem is retention, not recall; look at the in-office experience, hygienist continuity, and whether patients feel valued during visits; your reputation management data (reviews, ratings, feedback themes) can surface what’s driving attrition |
A useful diagnostic question: are patients not hearing from you, or are they hearing from you and choosing not to come back? The first is a recall system problem. The second is a practice experience problem. The fix for each is very different, and conflating them wastes time and money.
If patient experience or retention is the deeper issue, a stronger recall system will just surface the problem faster—not solve it. Address the root cause first.
> Back to Table of Contents
Scripts and templates you can use today
These are based on language patterns that consistently perform well in dental recall outreach. Adapt the tone to match your practice’s voice.
Pre-appointment script (at checkout)
“Dr. [Team] wants to see you back in six months for your next cleaning. I have Tuesday the 15th at 9 a.m. or Thursday the 17th at 2 p.m.—which works better for you?”
Why it works: it assumes the appointment is happening (not “would you like to...”) and offers two specific options, which is easier to say yes to than an open-ended question.
Automated text message (first reminder, 28 days before)
“Hi [Patient Name], it’s time to schedule your next cleaning at . Book online here: [link] or reply YES and we’ll call you to find a time.”
Why it works: short, clear, two easy ways to respond. No guilt, no medical jargon.
Human follow-up call (non-responder)
“Hi [Patient Name], this is [Staff Name] from . I’m calling because your hygiene visit is coming due, and I wanted to help you find a good time before the schedule fills up. Do you have a preference for mornings or afternoons?”
Why it works: personal, helpful tone. Creates gentle urgency (“before the schedule fills up”) without pressure. Ends with an easy question that moves toward booking.
Reactivation message (60+ days overdue)
“Hi [Patient Name], this is [Staff Name] at . We haven’t seen you in a while and just wanted to check in. We’d love to get you back on track with your cleanings whenever you’re ready. Is there anything we can help with to make scheduling easier?”
Why it works: no guilt. Acknowledges the gap without judgment. Opens the door for the patient to share barriers (cost, schedule, anxiety) that the team can help address. For patients with cost concerns, practices that offer a dental membership plan have an additional tool to remove the insurance barrier entirely.
Recall effectiveness tracking template
Track these five numbers monthly to measure whether your recall system is improving:
| 1. |
Total recall messages sent (texts + emails + calls)
|
| 2. |
Patients who responded (replied, clicked, or called back)
|
| 3. |
Patients who booked (scheduled an appointment)
|
| 4. |
Patients who kept (attended the appointment)
|
| 5. |
Recall effectiveness rate (kept ÷ sent × 100) |
Review these numbers in a weekly 10-minute huddle. Look for where the biggest drop-off occurs—that’s where your next improvement should focus.
> Back to Table of Contents
Next steps
If your recall system is running but your hygiene schedule still has gaps, the issue is almost always in the workflow—not the technology. Start here: measure your recall effectiveness rate for one month, then use the five failure points to identify where the biggest drop-off occurs, and fix that one step first.
If you want help auditing your recall process or building a patient communication workflow that integrates with your dental SEO and paid advertising strategy, schedule a consultation with our team. We work with practices every day to close the gap between marketing investment and kept appointments.
FAQs
What is a good dental recall rate?
Most well-run dental practices target a recare rate between 80–90%, meaning that percentage of active patients return for their scheduled hygiene visits within the recommended interval. If your rate is below 75%, there are likely workflow gaps in your recall process. Tracking your recall effectiveness rate (kept appointments divided by recall messages sent) gives you a more actionable number to improve than the overall recare percentage alone.
How often should a dental office send recall reminders?
A sequence of 2–3 automated messages spread across the 4 weeks before a patient’s due date tends to perform well without feeling excessive. Start the first contact 28 days before the due date. If the automated sequence produces no response by the due date, a personal phone call is the next step. Sending too many messages in a short window or continuing automated outreach indefinitely tends to increase opt-outs rather than bookings.
Should I use text, email, or phone calls for dental recall?
The best approach uses multiple channels in sequence rather than relying on one. Text messages work well for initial reminders because of high open rates. Email allows more context and a direct booking link. Phone calls are most effective for patients who haven’t responded to digital outreach, especially those who are significantly overdue. Varying the channel across your sequence reaches patients through their preferred communication method.
How do I reactivate patients who are long overdue?
Patients overdue by 60 days or more typically need personal outreach rather than automated messages. A brief, non-judgmental phone call or personalized message that acknowledges the gap and asks if there’s anything the practice can do to make scheduling easier tends to convert well. Avoid guilt-based language. Focus on being helpful and removing barriers like scheduling difficulty, cost concerns, or dental anxiety. If three contact attempts over two weeks produce no response, move the patient to a longer-interval reactivation cycle rather than continuing to call.
What is a good pre-appointment rate for a dental practice?
Aim for 80% or higher of hygiene patients booking their next visit before they leave the office. Pre-appointment is the most effective way to reduce the size of your recall list because patients who are already scheduled never become overdue. If your rate is below 70%, improving this single step will have a larger impact on your hygiene schedule than any change to your recall messaging.
Why do patients ignore dental recall messages?
The most common reasons are message fatigue (too many automated texts that blend together), inconvenient timing (messages arrive when patients cannot act on them), friction in booking (having to call during business hours instead of scheduling online), and a lack of personal connection (automated messages feel impersonal). Patients also ignore reminders when they have unresolved concerns about cost, treatment recommendations, or past negative experiences. A personal follow-up call often uncovers these barriers where automated messages cannot.
How do I know if my recall system needs to be replaced?
Before replacing your software, check whether the real problem is the tool or the workflow around it. Most recall systems have the basic features needed to run an effective sequence. If your system can send texts, emails, and generate call lists on a schedule, the technology is likely adequate. The more common issue is that no one has configured the timing correctly, added a human follow-up step, or assigned someone to track outcomes. Fix the workflow first. If the system genuinely cannot support multi-channel sequencing or outcome tracking, then consider an upgrade.
How long should I keep trying to recall an overdue patient?
A practical cutoff is three personal contact attempts over two weeks after the automated sequence completes. If three calls produce no response, move the patient to a 90-day reactivation list where they receive one more personal outreach. After that, the patient enters a low-frequency annual check-in cycle. Continuing intensive outreach beyond this point rarely converts and can lead to opt-outs or negative perceptions of the practice. Focus your team’s time on patients who are more recently overdue, where conversion rates are significantly higher. |
|



 Dental recall systems fail when the process runs on autopilot and nobody watches what happens after the message goes out. Most dental practices have some version of a recall process: automated texts, postcards, maybe a phone call list. But having a recall system and having one that actually converts overdue patients into kept appointments are two different things. If your hygiene schedule has open holes, your recare percentage is slipping, or your “past due” patient list keeps growing, the problem almost certainly isn’t that patients forgot about you. It’s that your
Dental recall systems fail when the process runs on autopilot and nobody watches what happens after the message goes out. Most dental practices have some version of a recall process: automated texts, postcards, maybe a phone call list. But having a recall system and having one that actually converts overdue patients into kept appointments are two different things. If your hygiene schedule has open holes, your recare percentage is slipping, or your “past due” patient list keeps growing, the problem almost certainly isn’t that patients forgot about you. It’s that your 


