Is Your Front Desk Process Undermining Your Dental Marketing Results?
Posted on 1/29/2026 by WEO Media |
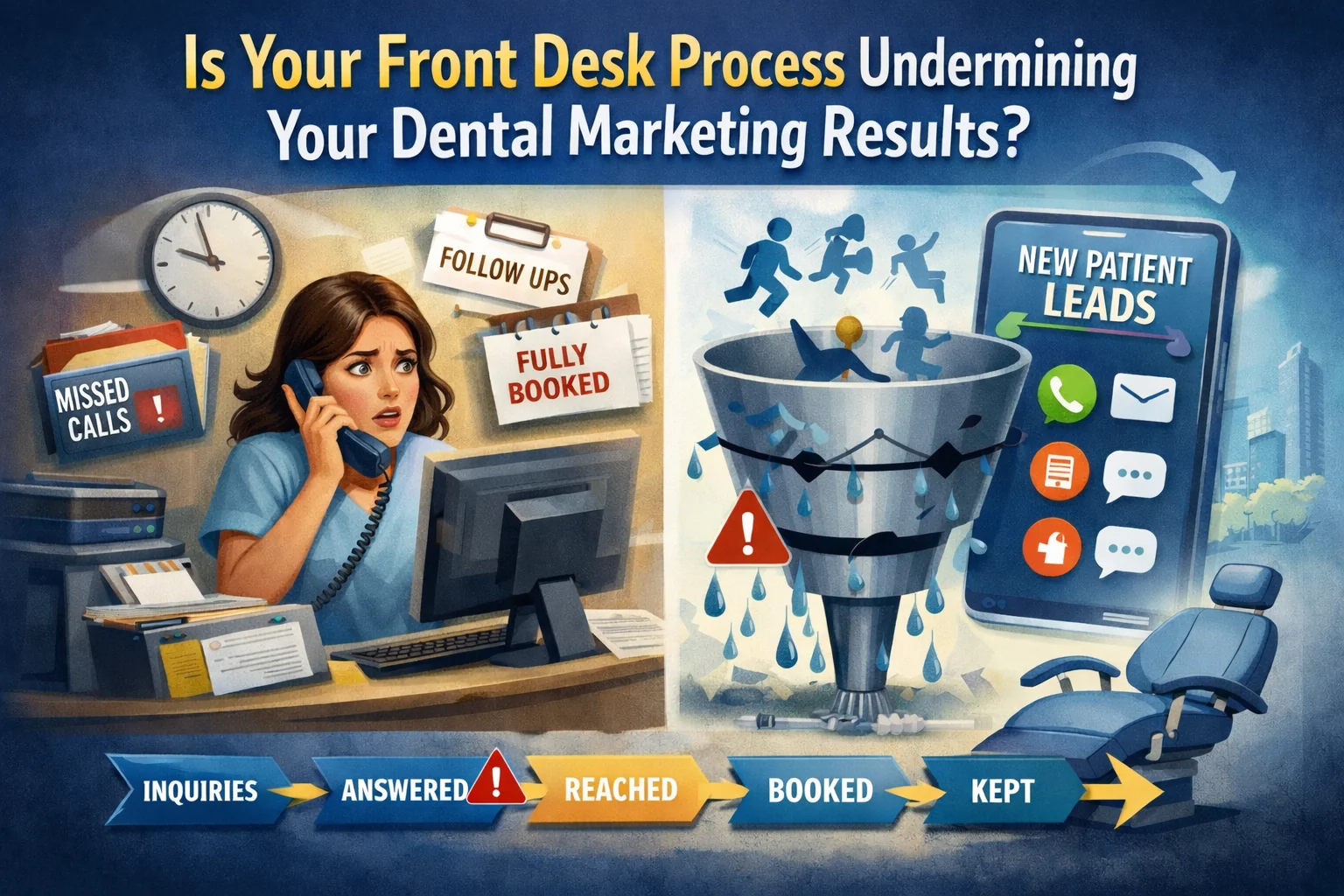
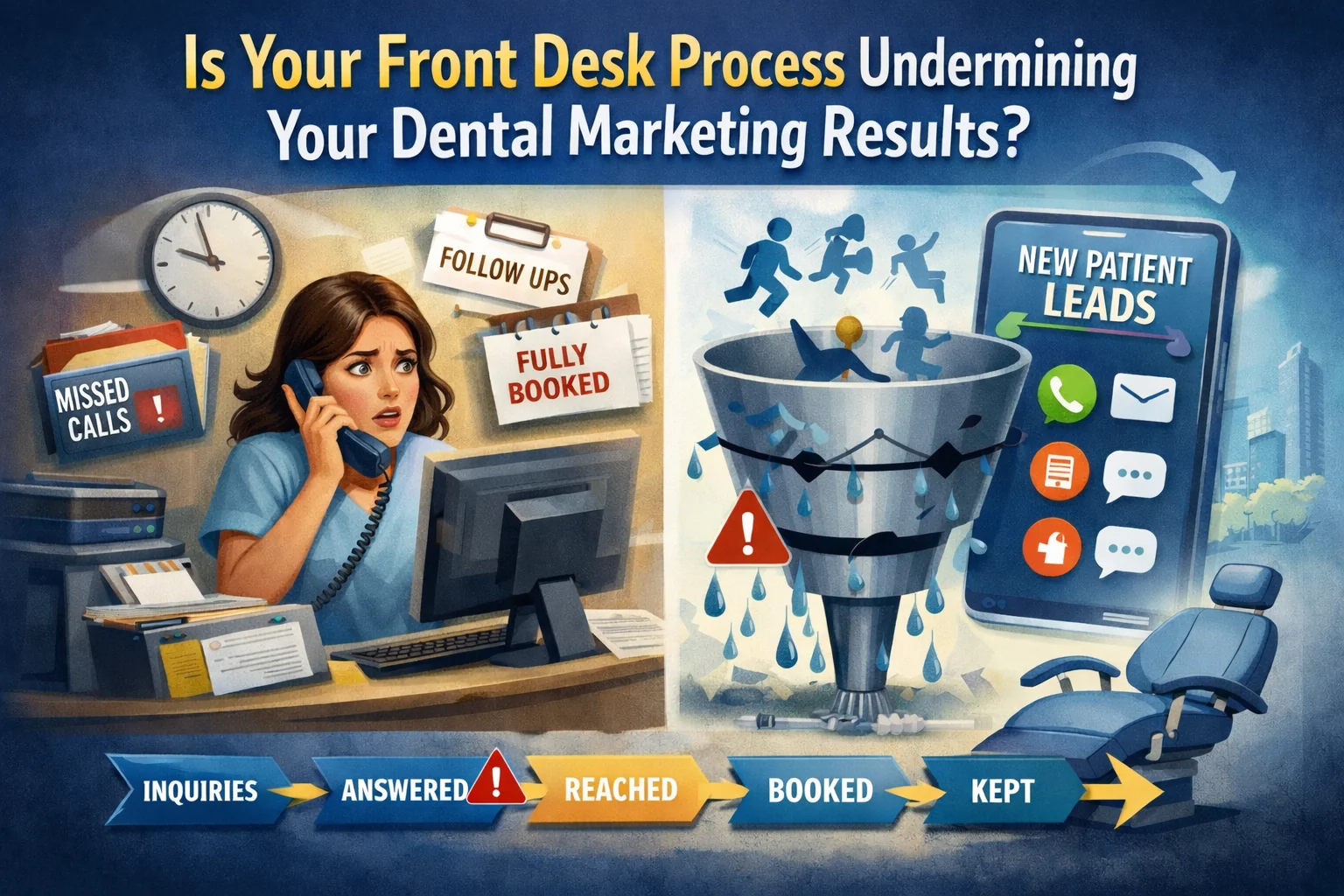 Yes—and it’s probably happening right now. If your marketing is generating calls, forms, and messages but your appointment book isn’t growing, the problem usually isn’t “bad leads.” It’s your intake process leaking demand before it converts. Yes—and it’s probably happening right now. If your marketing is generating calls, forms, and messages but your appointment book isn’t growing, the problem usually isn’t “bad leads.” It’s your intake process leaking demand before it converts.
The pattern is predictable: marketing drives interest, but somewhere between the first ring and the kept appointment, patients disappear. Whether your leads come from SEO, paid ads, or referrals, the intake process determines whether that investment converts. The four most common leaks are missed calls, slow follow-up, unclear booking permissions, and “booked-out” dead ends. These are system problems, not people problems—and they’re fixable.
Already generating leads? Keep reading. If lead volume is the issue, start with patient acquisition first.
Below, you’ll learn how to find exactly where the drop happens (inquiries → answered → reached → booked → kept) and fix it with coverage math, an outcome log, missed-call + scheduled callback SOPs, and copy/paste scripts—without blame or pressure tactics.
Written for: dental practice owners, office managers, and marketing teams who want to stop losing patients between the first call and the kept appointment.
TL;DR
If you only do five things, do these:
| • |
Answer the phones during peaks - protect coverage at lunch/end-of-day and use overflow so demand doesn’t vanish
|
| • |
Recover missed calls fast - one owner + due times + close-out rule so “not reached” doesn’t loop forever
|
| • |
Make booking possible - written permissions + simple visit types so the desk can book what marketing promotes
|
| • |
Stop arguing about lead quality - outcome logging separates spam/wrong intent from real workflow leaks
|
| • |
Use the scoreboard that matters - inquiries → answered → reached → booked → kept |
Table of Contents
How to measure your dental front desk conversion rate
If you’re skeptical of benchmarks or agency advice, use your own numbers to create proof in one week. You’re looking for where the drop happens—not who to blame.
In 7 days, document these five numbers: your answer rate
during business hours (answered ÷ total inbound calls during open hours), your reached rate (live answered + successful callbacks ÷ total inquiries), your booked rate (booked ÷ total inquiries), your kept rate (kept ÷ booked), and your top 5 friction notes—non-sensitive reasons patients stall, like “prefers Saturday,” “price-first,” “booked out,” “verification pending,” or “missed callback window.”
A simple “receipt” you can generate: pick one leak (like lunch-hour missed calls), implement one change (like a protected phone-first block + missed-call SOP), then compare week-over-week: answer rate, reached rate, booked rate, and kept rate. This turns “we think” into “we measured.”
Example (illustrative): Week 1: 210 inquiries → 62% answer rate → 71% reached → 44% booked.
Week 2 (after peak coverage blocks + missed-call SOP): 210 inquiries → 81% answer rate → 83% reached → 49% booked.
Results vary by staffing and capacity; this is a model for measuring impact.
> Back to Table of Contents
Start here in 5 minutes
| • |
Test peak-time phone handling - call at lunch and end-of-day; note answered vs missed, hold time, transfers, and whether a next-step appointment is offered
|
| • |
Test form routing - submit a test form; confirm the notification reaches the right person and a backup
|
| • |
Write one booked-out pathway - “next-best time + waitlist + scheduled callback” so calls don’t end at “we’re booked out” |
Write down your results: answer rate %, longest hold time, and whether staff offered a next-step appointment in the first 60 seconds.
> Back to Table of Contents
Leak Score self-assessment (5 questions)
Score 1 point for each “Yes” based on the last 7 days. Most practices score 2–3 on the first pass. That’s normal—it means you have the basics, but leaks are costing you appointments.
| 1. |
We protect phones during peak windows (named owner + backup during lunch/end-of-day/Mondays)
|
| 2. |
We respond fast to forms/messages during open hours (same day, with a named owner) and have a next-business-day after-hours plan
|
| 3. |
The person answering can book (no escalation for the top 3 promoted visit types)
|
| 4. |
We have an approved booked-out pathway (next-best time, waitlist, scheduled callback) used consistently
|
| 5. |
We track outcomes consistently (one owner, one final outcome) and review weekly without blame |
Interpretation:
> Back to Table of Contents
90-minute diagnostic worksheet (copy/paste)
☐ Peak-time phone test - call at lunch and end-of-day; record answered vs missed, hold time, transfers, and whether a next-step appointment is offered
☐ After-hours test - call after closing; note what voicemail asks for and the promised response window
☐ Form + message test - submit a test form/message; confirm the patient gets confirmation and the team gets alerts to a primary and backup
☐ Speed-to-lead check - measure time to first human response for a form/message
☐ Permissions check - confirm the answering role can book each promoted visit type without escalation
☐ Booked-out pathway check - ask for the earliest appointment; document whether alternatives are offered
☐ Start outcome logging - tag every inquiry for 7–14 days with intent + status + final outcome
Rollout rule: pick the single biggest leak you found and fix that first. Don’t roll out five new rules at once.
> Back to Table of Contents
Dental office phone benchmarks: answer rate, abandonment + speed-to-lead
Benchmarks should help you spot leaks—not start arguments. Treat these as internal directional targets you validate against your own call mix, staffing, and capacity.
| • |
Business-hour answer rate - many practices try to stay above ~85% when appropriately staffed; sustained under ~80% is a common red flag; fastest fixes are phone-first coverage blocks and overflow rules
|
| • |
Speed-to-lead for forms/messages - same day during open hours when feasible; assign a named owner and two daily “clear the queue” blocks
|
| • |
Missed-call recovery - same-day callbacks when possible; if you’re “waiting for them to call back,” write the SOP and track completion |
What is a good call abandonment rate? Abandonment is a friction signal, not a morality score. High abandonment usually points to one of four issues: holds are too long, the phone tree is too hard, transfers are too frequent, or peak coverage is too thin.
Fast fixes that often reduce abandonment:
| • |
Reduce transfers - capture intent + contact first, then route
|
| • |
Shorten the new-patient path - fewer menu steps, fewer dead ends
|
| • |
Offer scheduled callbacks - so patients don’t sit on hold
|
| • |
Make callbacks recognizable - set a window and use consistent caller ID when possible |
> Back to Table of Contents
Dental front desk phone coverage: staffing math that works
Coverage improves when it’s treated like math instead of a personality issue.
| • |
Coverage inputs - peak calls/hour and average handle time
|
| • |
Simple logic - when peak calls/hour × handle time approaches the hour, one person can’t reliably do phones plus check-in/out, walk-ins, and interruptions
|
| • |
Add buffer - checkout tasks and walk-ins steal phone time; overflow is what protects answer rate
|
| • |
Phone-first blocks - 2–3 blocks per day (30–60 minutes) often stabilize peaks more than coaching alone
|
| • |
Overflow rule - when primary is tied up, calls route to a trained backup or an answering service with a defined capture plan |
Illustrative example: peak volume 12 calls/hour × 4 minutes average handle time = 48 minutes of talk time per hour, before transfers and interruptions. That typically requires protected phone-first coverage during peaks plus a backup plan.
Two practical coverage patterns:
| • |
Small team (one primary desk person) - protect phones 11:30–12:30 and 3:30–4:15; a named backup covers checkout and walk-ins during those blocks
|
| • |
Two-person desk - rotate phone-first coverage at lunch and end-of-day so one person stays on calls while the other handles walk-ins and checkout |
> Back to Table of Contents
How to track dental lead outcomes (and stop blaming marketing)
Multi-touch journeys are normal: someone calls, submits a form, then texts. Without rules, you double-count and blame the wrong thing.
Status vs final outcome: use Status while you’re still working the lead (attempts, verification pending, callback scheduled). Use Final outcome once—when the lead is closed—and keep that one final outcome for reporting.
| • |
One lead, one owner - the person who creates the entry owns it until booked or closed
|
| • |
One identifier - usually phone number (or email) to merge duplicates
|
| • |
One final outcome - booked, not reached (closed), scheduled callback, wrong intent, spam/duplicate, policy mismatch, booked out, out-of-area
|
| • |
Weekly review - outcome mix + top friction notes, then choose 1–2 fixes for next week |
PHI-safe friction notes examples: “prefers mornings,” “price-first,” “verification pending,” “booked out,” “missed callback window,” “asked for Saturday.”
If you’re multi-location: include a location field and a single “home location” rule so leads don’t ping-pong between offices. One lead should live in one place. Read More: How DSOs Should Structure Their Marketing Teams for Scalable Growth
Copy/paste outcome log fields (minimal):
| • |
Date
|
| • |
Channel - call, form, text, chat, DM
|
| • |
Location (if applicable)
|
| • |
Intent - emergency eval, new patient, consult, existing patient, other
|
| • |
Status - attempt 1/2/3, callback scheduled, verification pending (optional)
|
| • |
Final outcome - booked, not reached (closed), scheduled callback, wrong intent, spam/duplicate, policy mismatch, booked out, out-of-area
|
| • |
Friction note - short, non-sensitive operational note
|
| • |
Owner - initials or role
|
| • |
Next action - call back, text back, verify, waitlist offer, close out
|
| • |
Due time - when the next action must happen |
Sample completed entries (sanitized):
| • |
Call - Intent: new patient; Status: callback scheduled; Final outcome: scheduled callback; Friction note: “prefers 2–3pm”; Due time: 2:15pm
|
| • |
Form - Intent: consult; Status: attempt 1 completed; Final outcome: not reached (closed); Friction note: “no answer”; Due time: next business day 9:30am
|
| • |
Call - Intent: emergency eval; Status: booked; Final outcome: booked; Friction note: “evaluation requested”; Due time: same day |
> Back to Table of Contents
Missed-call recovery + scheduled callback SOP
Missed calls don’t ruin growth—missing recovery does. Use one owner rule and one final outcome rule so missed calls don’t disappear.
| 1. |
0–5 minutes - create the lead entry; assign owner; set due time; Status: attempt scheduled
|
| 2. |
5–30 minutes - attempt 1 call back; if no answer, leave a minimal voicemail; Status: attempt 1 completed
|
| 3. |
30–120 minutes - attempt 2 call back; if texting is used, follow your consent policy and keep content non-sensitive; Status: attempt 2 completed
|
| 4. |
Same day (late afternoon) - attempt 3 call back; Status: reached or attempt 3 completed
|
| 5. |
Next business day (early) - final attempt; then close out; Final outcome: not reached (closed) if never reached |
Close-out rule: after the final attempt, set Final outcome = Not reached (closed) and stop recycling the same lead.
Scheduled callback option (high pickup rate):
| • |
Offer a window - “We can call you between 2:00 and 2:30 today—does that work?”
|
| • |
If they don’t answer - one retry inside the window, then reschedule a new window
|
| • |
Document it - Status: callback scheduled; Due time: start of window |
Minimal voicemail (privacy-aware): “This is the dental office returning your call. Please call us back at this number.”
Practical after-hours workflow: set expectations clearly and keep messages minimal. Example: “Leave your name and number and we will return your call the next business day.”
> Back to Table of Contents
Booking permissions + provider-controlled schedules
If your team reaches patients but still can’t book, the next bottleneck is usually permissions and visit types—not scripts.
Two operational options when providers tightly control the schedule:
| • |
Option 1: Pre-approved booking lanes - define 2–3 visit types marketing promotes and give the desk permission to book them without escalation
|
| • |
Option 2: Evaluation-first pathway - allow a short evaluation visit type that the desk can book, then clinical team controls next steps afterward |
Rule of thumb: don’t run ads for a visit type the desk cannot reliably schedule.
> Back to Table of Contents
Dental front desk phone script examples (copy/paste)
These scripts are guardrails you can personalize. The goal is consistent steps: intent, empathy, next step, booking, contact capture, and expectations.
How to use these: don’t read them word-for-word. Train your team on the structure (ask intent → acknowledge → offer next step → capture contact → set expectations), then let them adapt the language to sound natural.
Quick reference:
Script 1: New patient inquiry
Front desk: “Thanks for calling. Are you an existing patient with us, or are you looking to become a new patient?”
If new patient: “Great—how can we help today?”
Guide: “The next step is to reserve a visit so the doctor can evaluate and recommend options. I can schedule that for you. What days and times work best?”
Capture contact: “In case we get disconnected, what’s the best number to reach you?”
Expectations: “We’ll confirm your appointment and send reminders.”
Script 2: Emergency or pain (evaluation-first, no guarantees)
Front desk: “I’m sorry you’re dealing with that. The quickest next step is an evaluation so the doctor can assess and discuss options.”
Book: “We have an evaluation opening this week. Would a morning or afternoon work better?”
Expectations: “Treatment timing depends on what we find, but we can get the evaluation scheduled.”
Safety note: If symptoms feel severe or urgent, contact local urgent care or emergency services.
Script 3: Insurance-first caller (verification guardrails)
Front desk: “We work with many plans, and benefits vary by plan details. If you share your plan name and member information, we can verify benefits before giving plan-specific answers.”
Book-first option: “We can reserve the appointment now and complete verification before your visit. What day and time works best?”
Boundary: “I don’t want to guess on coverage, so we verify before confirming plan-specific details.”
Script 4: Price-first caller (efficient + next step)
Front desk: “I can help. Are you asking about the first visit, or a specific treatment?”
Expectations: “Exact fees depend on what the doctor finds, so the most accurate path is an evaluation.”
Capture contact: “In case we get disconnected, what’s the best number to reach you?”
Next step: “I can reserve an evaluation visit for you. Would you prefer mornings or afternoons?”
If they hesitate: “If you’d like, I can reserve the next-best time now and we can adjust if needed.”
Script 5: Booked out (no dead ends)
Front desk: “Our next available is Tuesday at 10:10am. I can reserve that now, and we can add you to a waitlist for earlier openings.”
Offer choice: “Would you prefer mornings or afternoons if we can move you up?”
Backup option: “If you’d like, we can set a scheduled callback window to finalize booking when you’re free to decide.”
Script 6: Existing patient accidentally routed as a “new patient”
Front desk: “Thanks for calling. Just to confirm—are you an existing patient with us?”
If yes: “Got it. I’ll get you to the right team. Before I transfer, what’s the best number in case we get disconnected?”
Transfer: “One moment—I’m connecting you now.”
Two phrases to avoid (trust-preserving):
| • |
Avoid: “We can’t help with that.” Use: “Here’s the next-best step we can offer.”
|
| • |
Avoid: “It’s not covered.” Use: “Benefits vary, so we verify your plan details before confirming coverage.” |
> Back to Table of Contents
Booked-out pathways + waitlist blueprint
If you can’t offer earlier appointments than competitors, you can still convert ethically by reducing uncertainty and offering a clear path.
| • |
Pathway 1: Next-best time + waitlist - book a real time today, then try to move them up
|
| • |
Pathway 2: Evaluation-first clarity - if only evaluation is possible, say so plainly and avoid implying treatment guarantees
|
| • |
Pathway 3: Scheduled callback - use a defined callback window when the patient needs time to decide |
Waitlist that actually works:
| • |
Minimum fields - best number, visit type, earliest acceptable date, day/time preference, notice required, contact method
|
| • |
Prioritization rule - first by short-notice readiness, then by urgency level, then by date added
|
| • |
Backfill workflow - offer the slot to best matches with a short response window, then move to the next
|
| • |
Exit rule - if a patient declines twice, confirm whether they still want to stay on the list |
> Back to Table of Contents
Call QA coaching (introduce it without fear)
QA works when it feels like training, not surveillance.
How to roll it out:
| • |
Tell the team what QA is for - consistency, fewer dead ends, easier days—not punishment
|
| • |
Start small - keep it manageable and repeatable
|
| • |
Coach behaviors, not personality - “captured intent” and “offered a next step” are coachable
|
| • |
One improvement per week - people adopt changes when they’re stable
|
| • |
Share wins - highlight one “good save” each week to keep morale up |
A simple behavior-based rubric (copy/paste categories):
| • |
Intent captured
|
| • |
Contact captured
|
| • |
Next step offered within first minute
|
| • |
Correct visit type chosen
|
| • |
Booked-out pathway used when needed
|
| • |
Insurance/pricing boundaries respected
|
| • |
Clear expectations set
|
| • |
Professional, calm tone
|
| • |
Accurate documentation (non-sensitive)
|
| • |
Closed-loop follow-up scheduled when not booked |
> Back to Table of Contents
Call tracking + attribution basics
Attribution gets messy when you mix existing-patient calls, duplicate leads, and multiple channels without one system.
Start with these basics:
| • |
Separate new-patient intent from existing-patient calls - ask “existing or new?” early and tag accordingly
|
| • |
Define what counts as a response - a live answer or successful callback counts; a voicemail-only attempt is not the same as a conversation
|
| • |
Prevent double counting - merge by identifier (phone/email) across calls, forms, and texts
|
| • |
Keep marketing tools clean - store operational outcomes without PHI; report campaigns in aggregate
|
| • |
Be deliberate with tracking numbers - if you use tracking on listings, have a clear NAP consistency strategy (don’t improvise); if you’re unsure whether your listings are consistent, run a local SEO audit to verify |
Make callbacks more likely to be answered:
| • |
Offer scheduled callback windows so patients expect the call
|
| • |
Set expectations - “We’ll call you between 2:00–2:30pm today”
|
| • |
Use consistent caller ID when possible
|
| • |
Document the window so it doesn’t disappear |
For step-by-step guidance, see Essential Guide: GA4 for Dental Websites
> Back to Table of Contents
Minimum viable tech stack
You don’t need a complicated CRM to run a reliable intake system. Minimum viable setup:
| • |
Phone reporting that shows inbound volume, answered vs missed, and abandonment/hold time if available
|
| • |
A shared outcome log with owner rules and close-out rules
|
| • |
PMS scheduling rules for promoted visit types (so the desk can book without escalation)
|
| • |
Two daily “clear the queue” blocks for forms/messages
|
| • |
Access control so only the right roles can see call recordings/logs (and nothing contains PHI in marketing tools) |
> Back to Table of Contents
Kept-rate protections
If you’re booking but not keeping, tighten expectations and reminders before blaming lead quality.
| • |
Confirmations - confirm appointment details and what to expect at the first visit
|
| • |
Reminder cadence - a short sequence that fits your practice style (for example: a confirmation shortly after booking, a reminder the day before, and a day-of reminder)
|
| • |
Clear next steps for reschedules - a simple path to reschedule without disappearing
|
| • |
Booked-out backfill - use the waitlist to fill cancellations quickly |
A smooth intake experience doesn’t just convert leads—it sets the tone for reviews and referrals.
> Back to Table of Contents
Privacy + compliance guardrails (US-focused)
This is a conservative operational approach, not legal advice. Disclosure wording and consent rules vary by state and circumstance, so confirm requirements with counsel and your vendors. This section is a risk-reduction checklist, not a legal determination of HIPAA/TCPA obligations.
| • |
Call recording disclosure - use a consistent approach; if a caller objects, follow your written policy
|
| • |
SMS safer defaults
- obtain consent where required, keep content non-sensitive, include opt-out for recurring messages, and limit frequency
|
| • |
Voicemail boundaries - keep messages minimal and avoid sensitive details
|
| • |
Retention and access - restrict access by role and define a retention period
|
| • |
PHI guardrail
- avoid including PHI in marketing tools, missed-call texts, or general logs |
> Back to Table of Contents
Want this implemented with you?
If you want help turning this into a running system (not a one-time checklist), we can build it with your team. We do not review PHI and do not provide legal or clinical advice—this is operational workflow work.
Typically you’ll see answer/reach improve first; timing varies by staffing and capacity.
What we do (and don’t) need to do this responsibly:
| • |
We need - high-level call patterns, schedule constraints, visit types, lead sources, and operational workflows
|
| • |
We do not need - patient medical details or protected health information for marketing analysis
|
| • |
We can work with redacted materials - focus is on routing, timing, categories, and system behaviors |
What you get:
| • |
Coverage plan - peak blocks + overflow rules tailored to your hours and volume
|
| • |
Outcome governance - categories, owner rules, close-out rules, and a weekly review routine
|
| • |
SOP pack - missed-call recovery, scheduled callbacks, and booked-out pathways
|
| • |
Scripts + QA rubric - copy/paste scripts and a coaching scorecard that stays fair
|
| • |
Closed-loop reporting - a weekly view that connects lead sources to booked and kept outcomes |
Example outputs you can expect (redacted style):
| • |
Routing map summary - “New patient calls route to Line A; overflow routes to Backup B; after-hours sets next-business-day callback expectation”
|
| • |
Outcome definitions excerpt - “Booked-out means no acceptable next-best time offered; Scheduled callback means a confirmed window with due time”
|
| • |
Weekly scorecard view - “Inquiries → reached → booked → kept, plus top 5 friction notes and the one fix for next week” |
> Back to Table of Contents
FAQs
What is a good answer rate for a dental front desk?
Many dental practices aim for an 85% or higher answer rate during business hours when appropriately staffed. Sustained rates below 80% often signal a coverage issue during peak windows like lunch, end-of-day, or Monday mornings. The fastest fixes are usually phone-first coverage blocks and overflow routing to a trained backup.
What is a good call abandonment rate for a dental office?
Abandonment rate is a friction signal, not a fixed benchmark. High abandonment usually points to holds that are too long, a phone tree that is too complicated, too many transfers, or thin coverage during peaks. Reducing transfers, shortening the new-patient path, and offering scheduled callbacks are common fixes that lower abandonment.
How do I calculate my dental front desk conversion rate?
Track four numbers over 7 days: answer rate (answered ÷ total inbound calls during open hours), reached rate (live answered + successful callbacks ÷ total inquiries), booked rate (booked ÷ total inquiries), and kept rate (kept ÷ booked). This shows exactly where patients drop off in your intake funnel.
Why are my dental marketing leads not converting to appointments?
The most common reasons are missed calls during peak hours, slow follow-up on forms and messages, front desk staff lacking permission to book promoted visit types, and “booked-out” responses with no alternative offered. These are system problems, not lead quality problems, and they are fixable with coverage rules, outcome logging, and clear booking permissions.
How quickly should a dental office return a missed call?
Same-day callback is the goal, with the first attempt ideally within 5–30 minutes of the missed call. A structured recovery SOP with defined attempt windows, owner assignment, and a close-out rule after the final attempt prevents missed calls from looping indefinitely or being forgotten.
What should a dental front desk say when the schedule is booked out?
Never end the call at “we’re booked out.” Instead, offer the next-best available time, add the patient to a waitlist for earlier openings, and ask their preference for mornings or afternoons if a slot opens. This keeps the patient engaged and gives them a clear path forward.
How do I stop my dental team from blaming lead quality?
Implement outcome logging with defined categories like booked, not reached, wrong intent, spam, policy mismatch, and booked out. When every inquiry gets a final outcome and weekly reviews focus on fixing the top friction categories, the conversation shifts from blame to process improvement.
What is speed-to-lead and why does it matter for dental practices?
Speed-to-lead is the time between when a patient submits a form or message and when they receive a human response. Same-day response during open hours is the target. Assigning a named owner and scheduling two daily “clear the queue” blocks helps ensure forms and messages do not sit unanswered.
Should my dental front desk be able to book appointments without asking the doctor?
For the visit types your marketing promotes, yes. If the front desk cannot book a new patient exam, cleaning, or evaluation without escalation, you will lose patients who call ready to schedule. Define 2–3 pre-approved booking lanes or use an evaluation-first pathway the desk can always offer.
How do I introduce call QA coaching without scaring my dental team?
Frame QA as training for consistency and easier days, not surveillance or punishment. Start with a small sample, coach observable behaviors like “captured intent” and “offered a next step,” focus on one improvement per week, and share wins by highlighting a good call each week. This builds trust and adoption. |
|



 Yes—and it’s probably happening right now. If your marketing is generating calls, forms, and messages but your appointment book isn’t growing, the problem usually isn’t “bad leads.” It’s your
Yes—and it’s probably happening right now. If your marketing is generating calls, forms, and messages but your appointment book isn’t growing, the problem usually isn’t “bad leads.” It’s your 


